
Buckle up… because what you are about to embark on is a comprehensive guide for 14 reasons for Missed Periods and why your period is late. If your periods are often late or you don’t know when they’ll come to visit, you are suffering from irregular cycles. I know it can feel overwhelming at times. Know that you don’t have to do this alone, support is just a click away. But education and knowledge can also feel empowering and give you back a sense of control and that is what I have intended to do in this thorough guide.
This article below is the thorough guide, however, if you’d like the slim version, more like a checklist of the 14 reasons for missed periods, please feel free to download the PDF here.
Understanding Your Menstrual Cycle: A Hormonal Perspective
You are supposed to have a period!
Your period and menstrual cycle are more than just a monthly event; it’s a vital sign of your hormonal and overall health. Think of it as your body’s signal, similar to a canary in a coal mine, indicating how well your health is functioning. When your period goes missing, it’s your body’s way of waving a red flag, urging you to pay attention and take action.
The Hormonal Symphony of Your Menstrual Cycle
Your menstrual cycle is orchestrated by a delicate interplay of hormonal events, spanning from one period to the next. The events of your menstrual cycle are broken down like this:
- Period: This marks the beginning of your cycle, characterised by the shedding of the uterine lining.
- Follicular Phase: From Day 1 of your period to ovulation, lasting 7-21 days, during which follicles in your ovaries mature and produce oestrogen.
- Ovulation: A brief moment when an egg is released from the ovary.
- Luteal Phase: Post-ovulation – from the day after ovulation to the day before your next period, lasting 10-16 days. The luteal phase prepares your body for a potential pregnancy. If pregnancy doesn’t occur, the uterine lining sheds, and the cycle begins anew. **Outside of pregnancy, it is not possible for your luteal phase to be longer than 16 days as the length is determined by the lifespan of the corpus luteum.
For a more thorough review of The Menstrual Cycle: The Phases and the Hormones, please visit my previous article here.
Normal Cycle Length: 21-35 Days
While textbooks may suggest a 28-day cycle, the reality is that most of us show individual variations.
A healthy menstrual cycle falls within the range of 21-35 days.
If your cycle spans 35 days, your period might seem late, but it could be normal for you.
To recap on “What is a Healthy Period”, please visit my previous article where is discussed the 9 signs and symptoms of a healthy, normal period.
What’s Happening Hormonally When Your Period Is Missing
Even though your period is the most noticed event of the four, the goal of every single menstrual cycle is ovulation, where the egg is released every month. And in order to get a period, you need to ovulate.
If you miss your period, two scenarios could be at play:
- Delayed Ovulation: A prolonged follicular phase leads to delayed ovulation. Despite this delay, ovulation still happens. Which means your luteal phase remains intact (10-16 days), resulting in a delayed period = long follicular phase with normal luteal phase length.
- Anovulation: Ovulation doesn’t occur, a condition known as anovulation. Without ovulation, there’s no luteal phase. Therefore, you are experiencing a long follicular phase that doesn’t achieve ovulation. You may eventually experience bleeding due to oestrogen-driven uterine lining growth. Note, this bleed isn’t technically a period
= a perpetual state of a follicular phase with no luteal phase.
Understanding these two hormonal scenarios helps us interpret the reason behind your missed period. By recognising these patterns, you gain valuable insights into your reproductive health, enabling you to make informed decisions about your well-being and possible treatment options.
Remember, your body speaks its own language; all it asks is for you to listen and adjust.
First Rule Out Pregnancy
At times, the most apparent causes aren’t necessarily related to hormonal imbalances, such as pregnancy and breastfeeding. While these situations are not caused by hormonal irregularities, I’ve included them for the sake of completeness and thoroughness.
Pregnancy: 🤰
It is first essential to rule out pregnancy, especially if sexual intercourse has occurred. If you’ve taken a pregnancy test and received a negative result, it’s important to note that it might be too early to detect HCG hormone levels. Another test in a few days could provide a more accurate result. Hence, before delving into other potential causes of your missed period, ruling out pregnancy is the crucial first step.
Breastfeeding: 🤱
Breastfeeding mothers often experience elevated levels of the hormone prolactin, which is crucial for milk production. These heightened prolactin levels play a significant role in suppressing or postponing ovulation. In some cases, this delay in ovulation can experienced for an extended period.
**Once pregnancy and breastfeeding have been ruled out, individuals with missed periods can generally be categorized into three groups:
- First-Time Occurrence or Occasional Missed Periods: If this is your initial experience with a missed period, or you’ve sporadically missed a couple, it might be a singular event.
- Irregular Menstrual Cycles: For those who have been experiencing irregular cycles and missing periods for a significant duration, recognising this pattern for a while has prompted the desire to understand the underlying causes.
- Sudden Awareness of Menstrual Irregularities: Some individuals may not have paid much attention to their menstrual cycles until now and have recently noticed their irregularity.
In these situations, there are several potential reasons for missed periods, delayed ovulation, or anovulation. Let’s get into these factors further, examining the 13 reasons why your period is late or missing periods. This exploration will serve as your compass, guiding you toward a comprehensive understanding of why your period might be missing. By uncovering these reasons, you’ll be empowered to seek an accurate diagnosis and, most importantly, receive tailored treatment.
14 Reasons for Missed Periods & Why Your Period could be Late
1. Stage of Life – Being a Teenager: 👧
As we discussed earlier, the standard menstrual cycle length for adults range from 21 to 35 days. However, for teenagers, a different timeline applies, especially when you are within 2-4 years of experiencing your first period.
During adolescence, the hormone system is still maturing. Consequently, the follicular phase, the time-frame leading up to ovulation, can be notably extended, sometimes up to 32 days. This prolonged follicular phase occurs because it takes longer for ovulation to happen while the hormonal system undergoes maturation.
For teenagers, a healthy menstrual cycle length can fall between 21 to 45 days. This broader range accounts for the natural variations in hormonal patterns during this developmental stage. If you find yourself within 4 years of your first period, your cycle could be delayed simply due to the fact that your hormone system hasn’t fully matured yet.
However, it’s crucial to note that if you haven’t started menstruating by the age of 16, it’s advisable to consult a healthcare professional. They can provide guidance and ensure there are no underlying issues causing the delay in your menstrual cycle.
2. Stage of Life – Perimenopause/Menopause: 🌅
Perimenopause is a natural phase of life when you are transitioning from your reproductive years towards the wisdom of menopause. Menopause, whether occurring naturally or through surgery (involving the removal of the uterus and ovaries), signifies the complete cessation of ovulation and periods.
During perimenopause though, which can span anywhere from 2 to 12 years, various symptoms may arise. These symptoms include hot flushes, night sweats, disturbances in sleep patterns, mood changes, heavier and prolonged bleeding, unexplained weight gain, and alterations in menstrual cycle length. Some women experience shorter cycles (less than 21 days), longer cycles, or missed periods, which is the focus of our discussion here.
A valuable insight into your own perimenopausal experience can often be gleaned from your mother’s journey. Asking her about her age when she entered menopause (as in period stopped and didn’t come back) provides a helpful reference point. Research indicates that daughters typically undergo menopause within a 5-year range of their mother’s experience, creating a 10-year window for your possible menopausal onset.
Studies conducted in 2004 and subsequent research have demonstrated a correlation between family history and menopausal age. Nearly half of the women surveyed entered menopause around the same age as their mothers. On average, daughters experienced menopause approximately one year earlier than their mothers. If early menopause occurred in the family, whether in a mother, sister, aunt, or grandmother, it often influenced the timing of menopausal onset in subsequent generations.
The average age of menopause is around 51, but perimenopausal symptoms can manifest up to 12 years before this milestone, starting as early as age 37. Therefore, if you’re in your late 30s and noticing changes in your menstrual cycle, perimenopause could be a significant factor. Engaging in open conversations with the amazing women in your family regarding their experiences can offer valuable insights.
If you are still in doubt, consulting your healthcare provider for a blood test can assess your proximity to menopause and help determine if perimenopause is the likely cause of your missed periods. This is more relevant if your menstrual cycles have been regular most of your menstruating life and now, moving into your wiser years, your cycles are changing.
3. Stress: 😓
Stress holds a profound influence on menstrual health, often underestimated in its impact. Within our bodies, the HPO axis—comprising the Hypothalamus, Pituitary Gland (our master controllers for reproduction), and Ovaries—orchestrates the delicate hormonal dance governing our menstrual cycles
Here’s how it works:
Hypothalamus and Pituitary Gland (Your Master Controllers for Reproduction):
When stress strikes, it directly targets the hypothalamus, reducing its hormonal signal (Gonadotropin Releasing Hormone or GnRH) to the pituitary gland. Consequently, pituitary hormones (FSH & LH) that communicate with the ovaries to encourage ovulation are diminished. In simpler terms, stress hampers the vital process of ovulation.
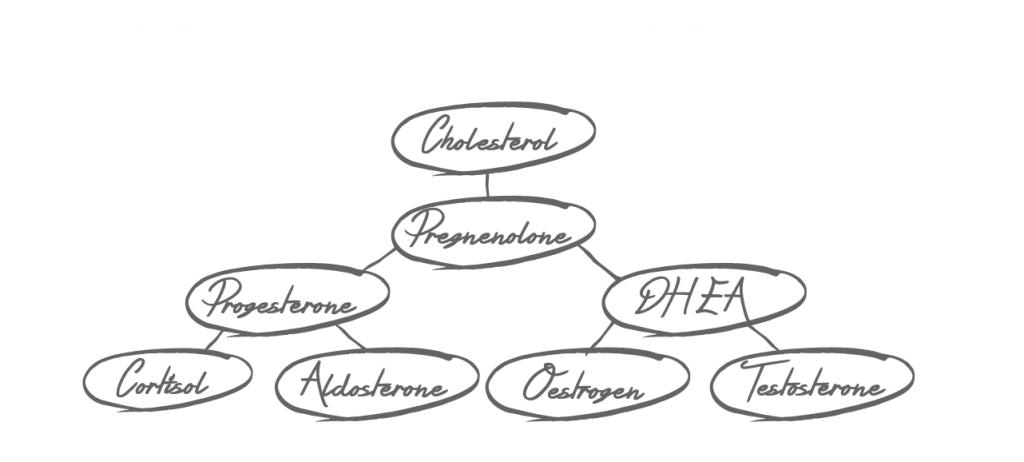
Hormonal Pathways: Understanding the Impact:
To understand the fertility-stress connection, consider the body’s hormone pathways. Cholesterol serves as the foundational block for all steroid hormones. Pregnenolone, derived from cholesterol, fuels the production of cortisol, oestrogen, and progesterone. In times of stress, the body prioritises survival (fight/flight responses) over reproduction. Hence, cortisol production takes precedence, often at the expense of reproductive hormones, especially progesterone, which aren’t deemed essential for immediate survival.
Recognising the Signs of Stress:
Irregular or missed periods can serve as visible markers of acute or chronic stress. Chronic stress can manifest in various ways, including PMS, low libido, fatigue, anxiety, depression, sleep disturbances, weakened immunity, low blood pressure, and imbalanced blood sugar levels.
Strategies for Managing Stress:
While relaxation techniques and enjoyable activities aid in stress management, addressing and minimising stressors becomes paramount. Life events like moving, marriage, exams, work-related stress, conflicts, financial pressures, job changes, divorce, relationship endings, or bereavement can all trigger stress. Recognising, managing, and, where possible, eliminating these stressors are pivotal steps in restoring hormonal balance and promoting overall well-being.
4. Illness: 🤒
An acute illness can affect the delicate balance of your body’s hormonal signals. When you’re ill, your hypothalamus detects the stress, prompting your body to channel its energy into healing and combating the infectious agent. This shift in focus temporarily alters hormonal signalling, often delaying or even preventing ovulation until your body regains its optimal functioning.
Here’s a closer look at how illness impacts your menstrual cycle:
Stress Response and Ovulation: Illness acts as a stressor, causing temporary changes in hormonal signalling, primarily during the follicular phase of your menstrual cycle. If illness strikes before ovulation, it can lead to delayed or inhibited ovulation. Once ovulation has occurred, it’s rare for your period to be missing or delayed solely due to illness.
Understanding the Body’s Priorities: Your body prioritises healing and restoration during illness, redirecting resources away from reproductive processes. This redirection is a natural response aimed at ensuring your overall well-being.
The Path to Recovery: As your body recuperates and returns to a state of balance, your menstrual cycle should resume its normal rhythm.
5. Circadian Rhythm Disruptions: 🌌
Circadian rhythm disruptions, a subtle yet impactful factor can dysregulate your hormones leading to menstrual irregularities. Disruptions in sleep, whether due to insufficient rest, frequent awakenings during the night, or the demands of shift work, register as stressors in your body. These stressors can also include too much blue light in the evening and not enough exposure to sun throughout the day. These stressors can lead to dysregulation of hormones, upsetting your circadian rhythm and affecting your menstrual cycle.
Shift Work and Irregular Cycles: Extensive research, conducted in 2011 and 2016, focused on women engaged in shift work. The studies revealed a significant correlation between prolonged shift work and irregular menstrual cycles. Women working shifts for more than 20 months were more prone to experiencing shorter cycles (less than 21 days) or longer cycles (exceeding 40 days). If you are a shift worker and your cycle surpasses 40 days, circadian rhythm disruptions could be a contributing factor. However, it’s crucial to explore other potential causes as well.
Impact of Travel: Even transient changes, such as crossing time zones during travel, can temporarily alter your menstrual cycle length, potentially causing you to miss a period.
6. Calorie Restriction: 🥗
Hypothalamic amenorrhea, a condition resulting in the cessation of periods, is closely linked to calorie restriction. When your body perceives a scarcity of energy due to limited calorie intake, the hypothalamus interprets it as an energy crisis. Consequently, vital functions take precedence, leading to the downregulation of hormones crucial for reproductive functions.
Stress on Reproductive Hormones: Calorie restriction triggers a state of energy scarcity. In response, the hypothalamus conserves energy by minimising the production of reproductive hormones, disrupting your menstrual cycle causing delayed ovulation or anovulation. This can result from undereating, extreme dieting, or eating disorders.
Body Fat Percentage: Maintaining a specific body fat percentage is essential for the regularity of your menstrual cycle. While individual factors vary, a body fat percentage below 15% often leads to missed periods. When your body falls below this threshold, the hormonal balance necessary for ovulation can be compromised.
Embracing Nutritional Balance: Recognising the significance of nourishing your body adequately is pivotal. Balanced nutrition, meeting your body’s caloric needs, supports the harmonious functioning of your reproductive system. Adequate caloric intake provides the energy essential for hormone production, fostering a regular menstrual cycle.
7. Excessive Exercise: 🏋️♀️
When intense exercise is coupled with calorie restriction and low body fat percentage, it often leads to anovulation, causing the absence of periods, sometimes persisting for several months.
Understanding the Impact of Extreme Exercise:
Reproductive Hormones Shutdown: In cases of extreme exercise (predominantly observed in dedicated athletes and women engaged in rigorous workouts), the body perceives the stress as a threat. In response, it reduces energy expenditure, leading to a shutdown of reproductive hormones. This adaptive mechanism prioritises survival over reproductive functions, causing missed periods.
Cortisol Disruption: Prolonged and intense exercise elevates cortisol levels, a stress hormone. Elevated cortisol interferes with the normal functioning of the hypothalamus and negatively impacts pituitary hormones like FSH and LH, crucial for follicle maturation and ovulation. Without ovulation, menstrual cycles are disrupted.
Recovery and Restoration: It’s essential to recognise that restoring hormonal balance after excessive exercise might take considerable time, even after weight gain and cessation of intense workouts. Patience and self-compassion are key during this healing process.
8. Nutrient Deficiencies: 🍎
All nutrients are essential for period hormones and health. There are some micronutrients, however, that are difficult to get in your diet depending on your food intake. Severe deficiencies in these micronutrients can disrupt reproductive hormones and ovarian function, potentially leading to missed periods.
Key Micronutrients and Their Impact:
Zinc: A crucial mineral that nourishes ovarian follicles, supporting healthy ovulation and progesterone production. Zinc deficiency may contribute to delayed ovulation, highlighting its significance in the menstrual cycle.
Vitamin D: Regulates hormone production of oestrogen and progesterone levels, which is essential for ovulation and maintaining a regular menstrual cycle.
Iodine: Directly influences oestrogen and ovulation. Iodine aids in the heatlhy processing and removal of oestrogen, ensuring the maintenance of oestrogen receptors. This intricate process promotes healthy ovulation.
Addressing Nutrient Deficiencies: When facing a missed period, it’s imperative to assess and address potential nutrient deficiencies.
9. Medications and Hormonal Contraceptives: 💊
Our bodies, intricate and unique, respond differently to medications. While not everyone taking specific medications experiences irregular or missed periods. Some medications have demonstrated effects on hormone levels, potentially disrupting the regularity of menstrual cycles. These medications encompass a range, including certain antidepressants, blood pressure medications, NSAIDs (non-steroidal anti-inflammatory medications), some antibiotics, chemotherapy drugs, and anti-seizure medications.
If you’ve observed alterations in your menstrual cycle while taking medications, it is important to consult your prescribing doctor on this one. A comprehensive discussion with your doctor can shed light on whether these medications impact your hormones and menstrual patterns.
Hormonal Contraceptives:
Hormonal contraceptives, such as the pill, patches, injections, or IUDs, inherently modify menstrual patterns, sometimes resulting in lighter or absent periods. These contraceptives shut down your body’s natural production of oestrogen and progesterone, replacing them with synthetic hormones that mimic your menstrual cycle. What may appear as a period during contraceptive use is essentially a withdrawal bleed, occurring due to the absence of synthetic hormones in the sugar pills.
10. Post-Pill Syndrome:
A phenomenon known as Post-Pill Syndrome emerges when menstrual cycles fail to resume after discontinuing hormonal contraceptives. This period of amenorrhea can persist for months or even years. The synthetic hormones in contraceptives temporarily shut down your internal hormonal communication system. For some individuals, it takes considerable time for this system to reboot naturally.
Not only will you have no periods, but you may also experience an absence of cervical fluid, especially the fertile egg-white kind. When this is the case, I often see low blood levels of FSH (the pituitary hormone) and low levels of oestrogen (from the ovaries). Low FSH can result from a history of taking hormonal contraceptives, fertility drugs or labour drugs such as syntocin.
Correct Diagnosis Matters:
Distinguishing between Post-Pill Syndrome and conditions like PCOS (Polycystic Ovary Syndrome) is crucial. Misdiagnosis could lead to inappropriate treatments, exacerbating irregular cycles. For example, some treatment options for PCOS could cause a swing from post-pill syndrome to hypothalamic amenorrhoea, further worsening hormone imbalances and long cycles.
11. PCOS (Polycystic Ovarian Syndrome): 💻
Irregular or missed periods often serve as the hallmark symptom of Polycystic Ovarian Syndrome, commonly known as PCOS. In this condition, hormonal imbalances disrupt the normal functioning of the ovaries, leading to a range of symptoms.
The Role of Testosterone: High levels of testosterone, often a key player in PCOS, exerts a significant influence. Elevated testosterone disrupts the essential processes of egg development and release from the ovaries. Consequently, ovulation becomes erratic, occurring at varying times throughout your menstrual cycle or, in some instances, not happening at all. This irregularity manifests as absent or irregular periods, forming a crucial part of the PCOS symptomatology.
In addition to menstrual irregularities, PCOS often presents an array of challenges, including weight gain, struggles with weight loss, unwanted body or facial hair, and high insulin levels, among others. These diverse symptoms collectively underscore the complex nature of PCOS.
The Importance of Accurate Diagnosis: A correct diagnosis is not just a formality; it is the linchpin upon which tailored, effective treatment strategies are built. To support you in this journey, consider exploring my PCOS diagnosis download. This valuable resource aligns with established PCOS diagnostic criteria, empowering you with clarity and helping you move closer to an accurate diagnosis.
12. Thyroid Disorders: 🦋
Within your intricate hormonal system, thyroid imbalances exert significant influence, capable of disrupting the delicate balance of reproductive hormones and leading to missed periods.
Hypothyroidism:
In this condition, your thyroid gland underperforms, and doesn’t produce sufficient thyroid hormone. Low thyroid hormone levels can result in various menstrual irregularities:
- Anovulation: Ovulation falters, leaving you with delayed or entirely missed periods.
- Amenorrhea: In severe cases, periods vanish for extended periods.
- Prolonged Menstrual Periods: Some experience heavier and longer bleeds, further complicating the cycle.
Beyond menstrual irregularities, hypothyroidism manifests in tell-tale signs such as fatigue, constipation, and intolerance to cold. If these symptoms accompany your absent periods, consulting your doctor for thyroid hormone evaluation is your first step.
In hypothyroidism, blood test results often show a high TSH, which indicates low thyroid function. High TSH can also elevate prolactin levels, which further inhibits progesterone production and ovulation.
The most common cause of hypothyroidism is auto-immune reasons, but other causes can be nutrient deficiencies, stress and/ or exposure to environmental toxins.
Hyperthyroidism:
On the flip side lies Hyperthyroidism, where your thyroid gland goes into overdrive, producing excessive thyroid hormones. The impact on your menstrual cycle is notable:
- Irregular Periods: Cycles become shorter and erratic, with periods occurring more frequently.
- Decreased Menstrual Flow: Periods become lighter and infrequent.
- Amenorrhea: Complete absence of periods.
Accompanying symptoms include a heightened metabolism, constant hunger, unusual warmth, excessive sweating, agitation, anxiety, and palpitations.
In blood tests, a low TSH (Thyroid Stimulating Hormone) signifies a hyperactive thyroid. Accompanying hyperthyroidism is often elevated testosterone levels, which we know can disrupt ovulation and cause missed periods.
Hyperthyroidism often arises from autoimmune disorders such as Graves’ disease or thyroid nodules that produce excess thyroid hormones, or it can also be exacerbated by inflammation.
Given these complexities, if your periods are irregular and you notice some of the other symptoms mentioned above, it’s essential to see your doctor to rule out thyroid disorders.
13. High Prolactin Levels: 🍼
Prolactin is particularly important for breastfeeding mothers as it is responsible for milk production. However, when prolactin surges, it can dampen the production of crucial hormones—oestrogen and progesterone—leading to suppressed ovulation and consequently, erratic or missed periods.
Causes of Elevated Prolactin:
Several factors could drive up your prolactin levels, disrupting your menstrual harmony:
- Breastfeeding: Even a few feeds a day can elevate prolactin, impacting your oestrogen and progesterone balance.
- Benign Pituitary Tumours: These growths on the pituitary gland can excessively secrete prolactin, necessitating pharmaceutical interventions.
- Hypothyroidism: Insufficient thyroid hormone levels can trigger prolactin spikes, further complicating your menstrual cycle.
- Stress: Prolactin can mirror cortisol, the stress hormone. During times of heightened stress, the surge in cortisol can drive up prolactin levels, disrupting your hormonal equilibrium.
Once again, accurate diagnosis forms the cornerstone of effective treatment. Your first step is consultation with your doctor for blood tests to investigate the possible causes.
14. Premature Ovarian Failure (POF) 🌸💔
Premature Ovarian Failure, a phenomenon similar to early menopause, unfolds when the ovaries lose their functional finesse before the age of 40.
Understanding Premature Ovarian Failure:
- Diminished Egg Quantity and Quality: POF results in a diminished reserve of eggs in the ovaries, coupled with a decline in their quality.
- Irregular Ovulation: The ovaries, no longer produce and release eggs regularly. Consequently, the ovaries then produce lower levels of oestrogen and progesterone, leading to irregular ovulation or its absence altogether.
- FSH Elevation: The compromised ovarian function triggers a surge in Follicle-Stimulating Hormone (FSH) secreted by the pituitary gland. Ordinarily, FSH nurtures the growth of ovarian follicles, yet the ovaries, now resistant, respond inadequately. This resistance translates into fewer mature follicles, hampered ovulation, and frequently missing periods.
Premature Ovarian Failure is challenging, but as we have explored in this comprehensive guide on 13 reasons why your period is late, there are 12 other reasons to rule out. Therefore, it is worth investigating with your healthcare practitioner and your doctor so you can arrive at a correct diagnosis.
Conclusion
Taking Control of Your Health
🌺 Seeking Medical Advice: If you’re experiencing irregular periods, consulting a natural healthcare practitioner and your doctor is crucial. Accurate diagnosis and personalised guidance can pave the way for hormonal balance and overall well-being.
Empowering Your Journey: Reclaiming Control
In this intricate dance of hormones and health, it might feel like your body has a mind of its own. Often times, you have more control than you think. Here’s your guide to reclaiming that control:
- Knowledge is Power: Understanding your body and menstrual cycle is the first step. Tracking your cycle can provide valuable insights, offer clues, and help you make informed decisions about your health and fertility.
- Harness the Power of Tracking: As always, my “Master Your Menstrual Cycle” online course is here to educate and empower you further. Click here to join the waitlist for the course. It’s an absolute comprehensive guide to Menstrual Cycle Tracking, equipping you with knowledge about your cycle, intimately understanding your fertile window and ovulation. These insights serve dual purposes: aiding in family planning and optimising your chances of conception.
Remember, one way your body communicates its needs is through your menstrual cycle. Listening and understanding can empower you on your journey to optimal health and fertility.
Here’s to understanding, empowerment, and the magic within you.✨✨
Amanda x
